As many of you know, this is Women’s Health Week. We wanted to take some time today to talk about colorectal cancer in women, risk factors, and how we can prevent it.
The typical lifetime risk of developing colorectal cancer is about 1 in 21 (or 4.7%) in for men and approximately 1 in 23 (or 4.4%) for women. (American Cancer Society) Yes, this means that, overall, women have a slightly lower risk of developing colorectal cancer than men. There are plenty of potential risk factors to consider, however, that could mean that a woman is not of “typical” or average risk.
There are two classifications of colorectal cancer risks: those that you can modify and change and those that you cannot.
Risks within your control include: 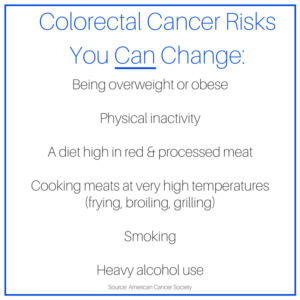 being overweight, being inactive, eating a diet high in red and processed meats, cooking meats at very temperatures (such as grilling, broiling, or frying), smoking, and using alcohol heavily.
being overweight, being inactive, eating a diet high in red and processed meats, cooking meats at very temperatures (such as grilling, broiling, or frying), smoking, and using alcohol heavily.
Great first steps to preventing colorectal cancer include achieving and maintaining a healthy weight and becoming more active. Whether you enjoy walking in your neighborhood, running, swimming, biking, playing frisbee, or anything else you might imagine, regular physical activity is an excellent prevention activity! Reducing your intake of red and processed meats is crucial as well, as is ensuring that you eat a diet rich in fruits, vegetables, and whole grains. (Fiber is your friend!) Reducing alcohol consumption is also key.
It’s important to control the risks you can. After all, there are many colorectal cancer risks beyond your control.
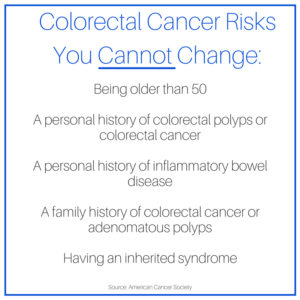 For example, you risk of developing colorectal cancer goes up after you turn 50. It’s important to know, however, that you may need to be screened before 50, depending on your personal risk.
For example, you risk of developing colorectal cancer goes up after you turn 50. It’s important to know, however, that you may need to be screened before 50, depending on your personal risk.
Other risk factors include personal and family histories of colorectal cancer and colorectal polyps. You need to talk to your family members about the results of their colonoscopies. If your mother or father had polyps removed at the age of 50, it is likely that your doctor will recommend early screening for you – perhaps as early as age 40. This might be an uncomfortable conversation (we talk about butts all day long and we understand that you might not!), but it’s a potentially lifesaving conversation to have.
In addition, having an inflammatory bowel disease like Crohn’s or Colitis also increases your risks. Finally, inherited syndromes, such as Lynch Syndrome or Familial Adenomatous Polyposis (among others) can increase not only your risks of colorectal cancer, but especially your risks of early-onset colorectal cancer. Your doctor may recommend genetic testing for you and other members of your family.
This genetic testing can reveal powerful information – and not just about colorectal cancer. For example, genetic testing might reveal that you have a BRCA 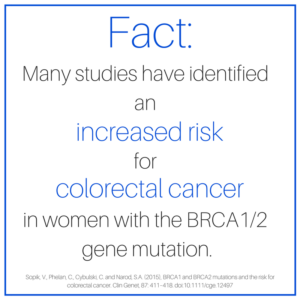 gene mutation. Individuals with a BRCA1 or BRCA2 gene mutation are at high risk of developing both breast and ovarian cancers. But these mutations may increase the risk of developing other cancers as well, including colorectal. If you have one of these mutations, your doctor should recommend early colorectal cancer screenings for you, since colorectal cancer can be effectively prevented through timely colonoscopy and removal of any precancerous polyps. Recent studies have shown that a BRCA1 mutation contributes to particularly high colorectal cancer risk in women under the age of 50, moreso than in women over the age of 50.
gene mutation. Individuals with a BRCA1 or BRCA2 gene mutation are at high risk of developing both breast and ovarian cancers. But these mutations may increase the risk of developing other cancers as well, including colorectal. If you have one of these mutations, your doctor should recommend early colorectal cancer screenings for you, since colorectal cancer can be effectively prevented through timely colonoscopy and removal of any precancerous polyps. Recent studies have shown that a BRCA1 mutation contributes to particularly high colorectal cancer risk in women under the age of 50, moreso than in women over the age of 50.
Based on this evidence, many experts recommend that women with these mutations receive colonoscopies at 3-5 year intervals, beginning at age 40, if not sooner. (Sopik, V., Phelan, C., Cybulski, C. and Narod, S.A.)
It is essential for you to know your family history. We may sound like a broken record, but we’re okay with that. In addition to that family history, however, it’s important that you know your own risks and the symptoms of colorectal cancer.
We’ve covered a lot of ground with this post, but here’s the rundown in a nutshell:
- Women have colons and rectums. (Yes, you do. If you don’t, you would definitely know it. They’re not just part of the “dude setup.” They are an integral part of every human digestive system.)
- If you have a colon and rectum (see above), you should screen it for colorectal cancer.
- Most standard colorectal cancer screenings begin at age 50, but this might NOT be soon enough for you.
- Knowing your family history and personal risks will help you and your doctor decide when you should be screened for colorectal cancer. It might be 50. It might be 29.
- Once you know your “number,” DON’T WAIT. If you should be screened at 50, get screened at 50. Don’t wait until 55 or 60. It might be too late.
Much of this information applies no matter your biological sex. We hope this has inspired you to assess your own personal risks, talk to your family members, and, most importantly, figure out when you should be screened!
Remember, colorectal cancer is extremely preventable, but in order to prevent it, you need to be screened. On-time screening saves lives. Pure and simple. So ladies, take care of yourselves and talk to your doctor about colorectal cancer screening. Everyone else? Show the women in your life how much you love them by reminding them to get screened. Remind them frequently if they are hesitant. They’ll thank you someday.
If you’re interested in reading the stories of women fighting colorectal cancer, many of these brave souls have taken to writing. Women’s Health and SELF magazine both promoted features for Colon Cancer Awareness Month. Enjoy.
Sources:
- American Cancer Society
- Sopik, V., Phelan, C., Cybulski, C. and Narod, S.A. (2015), BRCA1 and BRCA2 mutations and the risk for colorectal cancer. Clin Genet, 87: 411–418. doi:10.1111/cge.12497

You must be logged in to post a comment.