Thanks for tuning in as we continue our week-long blog series on why it is ESSENTIAL that we start talking about colon cancer before the age of 50. On Monday, we learned about Karen Walsh, a passionate advocate for colon cancer prevention and awareness. Karen is currently battling stage IV colon cancer and, in her keynote address at the National Colorectal Cancer Roundtable, asked why she (and so many fighters like her) had never been told the symptoms of colon cancer or that knowing your family history is important because it could effect the age at which you should be screened. (Hint: For many people, it must be earlier!) Yesterday, we hope we answered Karen’s questions (and maybe some of yours, too)!
So, we hope you’ve learned a lot so far this week. Namely that:
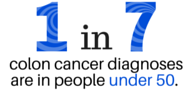
- 1 in 7 diagnoses of colon cancer are in people under the age of 50
- It is important to know the symptoms of colon cancer and talk to your doctor immediately if you experience any
- Knowing your family history is essential to determining when you should be screened
- Talking to your doctor before you turn 50 will give them the information they need to determine when you need to be screened
- ON-TIME SCREENING SAVES LIVES
 We know what you’re thinking – many providers don’t begin to talk about colon cancer with their patients until the patient turns 50. You may be one of those patients. We want to change this. Doctors follow guidelines set forth by organizations like the American Cancer Society and the American Heart Association, to name a few. The current recommendation is for a colon cancer screening age of 50.
We know what you’re thinking – many providers don’t begin to talk about colon cancer with their patients until the patient turns 50. You may be one of those patients. We want to change this. Doctors follow guidelines set forth by organizations like the American Cancer Society and the American Heart Association, to name a few. The current recommendation is for a colon cancer screening age of 50.
But as we’re seeing from the data, we’re missing an awful lot of people by waiting until 50. This is particularly obvious when you consider the fact that colon cancer in individuals under the age of 50 is increasing sharply.
We, the colon cancer community, must pivot our current position to an opportunity for inclusion – evidence based of course.
This is what we know now and what we should disclose to the public now.
- We know there is an alarming increase in colon and especially rectal cancers in the under age 50 age group. Soon 20% of all rectal cancers will occur under the age of 50.
- We know that to better tailor screening age, the accurate family history needs to be identified long before the age of 50 (preferably before but certainly by age 40) in order to deliver screenings to those most at risk due to genetic or familial factors.
- We know that due to a timely lack of awareness and understanding, most sporadic (non-genetic) cases of colon and rectal cancer occurring under the age of 50 have a significant delay in notification of the provider and then an additional delay in appropriate timely diagnosis once in the system. Patients and physicians are generally not aware of the dramatic increases. Many occurrences of colon and colorectal cancer in people under the age of 50 are misdiagnosed.
- We know that just over half of asymptomatic, normal risk individuals are screened anytime during their fifth decade because they know too little about the entire issue until they are or just after 50. This means that only half of those individuals are screened in their fifties – the other half wait.
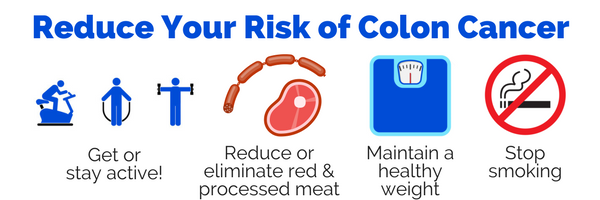
- We know that there are disease modifying behaviors that, if implemented, can reduce the risk of ever developing colon or rectal cancer, which also promote general good health BUT only when implemented early enough to count. Smoking cessation, dietary changes like avoiding red or processed meats, regular exercise, maintaining a healthy weight are but a few powerful, evidence-based risk reduction recommendations.
The Colon Cancer Prevention Project recommends a radical change in both thinking and action to address the longstanding, self-imposed embargo on evidence based, time sensitive information regarding colorectal cancer to those under the age of 50.
Specifically, we should give as much attention to this issue as we have to the audacious and successful 80 x 18 campaign.
The 80 x 18 campaign holds a goal of screening 80% of eligible individuals by the year 2018. It’s a great goal, but it is primarily focused at screening individuals at the currently recognized recommended screening age of 50.
We say that’s not good enough. In order to reach and screen more of those asymptomatic, normal risk individuals in the fifth decade, we need to begin the conversation earlier, say in the forties. For those individuals who are at risk, either due to family history, risk behaviors, or other potential cause, we need to begin the conversation MUCH earlier.
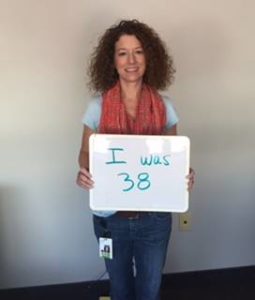
Karen Walsh was 40 when she was diagnosed with stage IV colon cancer. She didn’t know the symptoms. She didn’t know that the fact that her grandmother had colon cancer or that both of her parents had polyps removed put her at advanced risk. She hadn’t been told. How many Karens are there in the world who, as they fight their battle with colon cancer, can ask, “Why didn’t anyone tell me?”
That question haunts us. It should haunt everyone who works in healthcare, health advocacy, health education, or colon cancer specific outreach. Why didn’t  we tell them?
we tell them?
We’ve had enough. The evidence is clear – colon cancer is on the rise in individuals under 50 and we are doing them an immense disservice by not fighting to change the standards. We need to talk about colon cancer well before the age of 50. We need to talk to your families, our loved ones, to get a complete family history. We need to advocate for ourselves to our doctors. We need to fight to tell people about colon cancer.
Tomorrow, we’ll be discussing in greater detail what YOU can do to help make this change. We hope you’ll stick with us.
You must be logged in to post a comment.